Mental Health Among Veterans with ALS
If you are experiencing thoughts about ending your life, please Text HOME to 741741 to connect with a Crisis Counselor or call the National Suicide Prevention Lifeline at 1-800-273-8255 for free and confidential support now.
We’ll cut to the chase early — ALS can be scary, overwhelming and traumatizing. It also is life-changing. You’re not alone in experiencing feelings that question, “Why me?” and “Do I want to live with this?”
Breathe. You are not alone in feeling this way. Veterans are twice as likely to be diagnosed with ALS compared to their civilian counterparts. This means that you have a community that understands what you’re going through and can provide support and answers to the questions and worries you may have. You can connect with other veterans who are impacted by ALS here.
Emotional Impact of ALS:
Most often, ALS is something that never crosses a person’s mind until they are experiencing symptoms, being diagnosed or have a close relationship with someone who has been diagnosed. In turn, when a diagnosis does happen, it’s an extreme shock.
We are learning more about the heterogeneity of ALS every day — which means that ALS progresses differently in each person. The constant stress related to the uncertainty of what to expect, the physical and psycho-emotional changes and the lack of control associated with this can lead to experiencing trauma. “Trauma is not what happens to you, it’s what happens inside you as a result of what happened to you.”
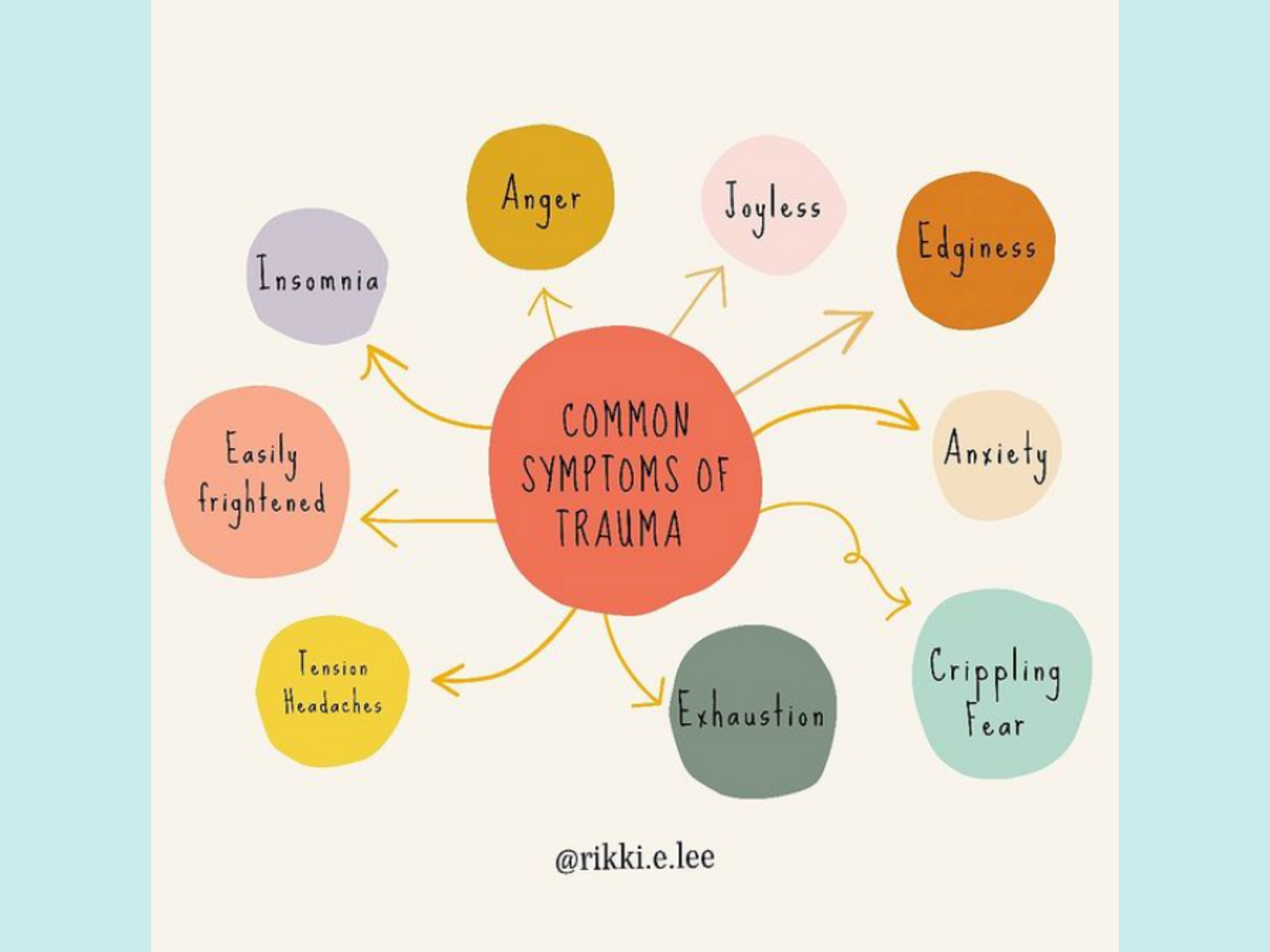
Trauma impacts our mental, emotional and physical health. It is the “invisible force” that shapes us and influences the way we view and interact with our surroundings. Trauma affects everyone differently. The impact of trauma can be subtle, gradual or outright destructive. It is also natural for these trauma responses to change over time.
For many, this could include feeling like the future is hopeless, that life will be less positive than it used to be and that good things, or even normal life events, won’t happen anymore. It is completely normal to have thoughts influenced in this way as a trauma response but it does not mean that those feelings and thoughts represent the truth about your current situation or future. Trauma is sort of like an outside entity taking over the section of your brain that controls your emotions, which changes the way you would normally think about things. These feelings are valid but they don’t have to last forever.
Overall mental health can also be impacted by trauma in how strongly a person feels (or disregards) their emotions. Traumatic stress tends to bring out two mental health extremes: feeling either too much (overwhelmed) or too little (numb) emotion.
On the physical side, trauma shows itself most often through something called a somatic complaint (this is when a person describes emotional stress through a physical ailment) — sleep disturbances; gastrointestinal problems, cardiovascular issues, neurological, musculoskeletal, respiratory and dermatological disorders; urological problems; and substance abuse issues or disorders.
It is important to note that not everyone may experience a trauma response to an ALS diagnosis.
Depression:
Depression. We hear this word used frequently in day-to-day life, but what does it really mean?
Depression is different from just having a few “bad” days or feeling some stressful emotions based on everyday life events. It’s a medical diagnosis classified as a mood disorder and it can affect anyone. It commonly shows up through repeated, longstanding feelings of intense sadness or hopelessness, losing interest or pleasure in activities that you used to enjoy, experiencing feelings of guilt, unworthiness or low self-esteem and the desire to avoid being around people.
People living with ALS are at high risk of being diagnosed with depression, especially leading up to and within the first year after diagnosis. Sometimes depression sneaks up on you. Here are some things to watch for in yourself or a loved one that may indicate you or they are experiencing depression:
- Feeling sad or hopeless.
- Losing interest in or not getting pleasure from most of your daily activities.
- Sleeping too much or not enough almost every day.
- Feeling tired or as if you have no energy almost every day.
- Significant changes to appetite leading to eating more or less than usual almost every day.
Depression can be the result of a few different cause factors but some of the most common are trauma, life events, medical conditions and brain structure.
While it is a very common mental health disorder, especially among veterans, it should be taken seriously and addressed with your healthcare provider. The good news is that even the most severe cases of depression are treatable and there are many methods and treatments available to help manage it.
To be treated for depression, you’ll need to visit a mental health professional for an evaluation and diagnosis. They will ask you a series of questions about topics such as moods, appetite, sleep pattern, thoughts and past traumas. Once a diagnosis is reached, you can work with your healthcare provider to create an effective treatment plan. This can include:
- Medications
- Counseling/Therapy
- Light Therapy
- Exercise Plan
- Self-Care
- Supplements/Vitamins, and more
Suicidal Ideation and Mental Health:
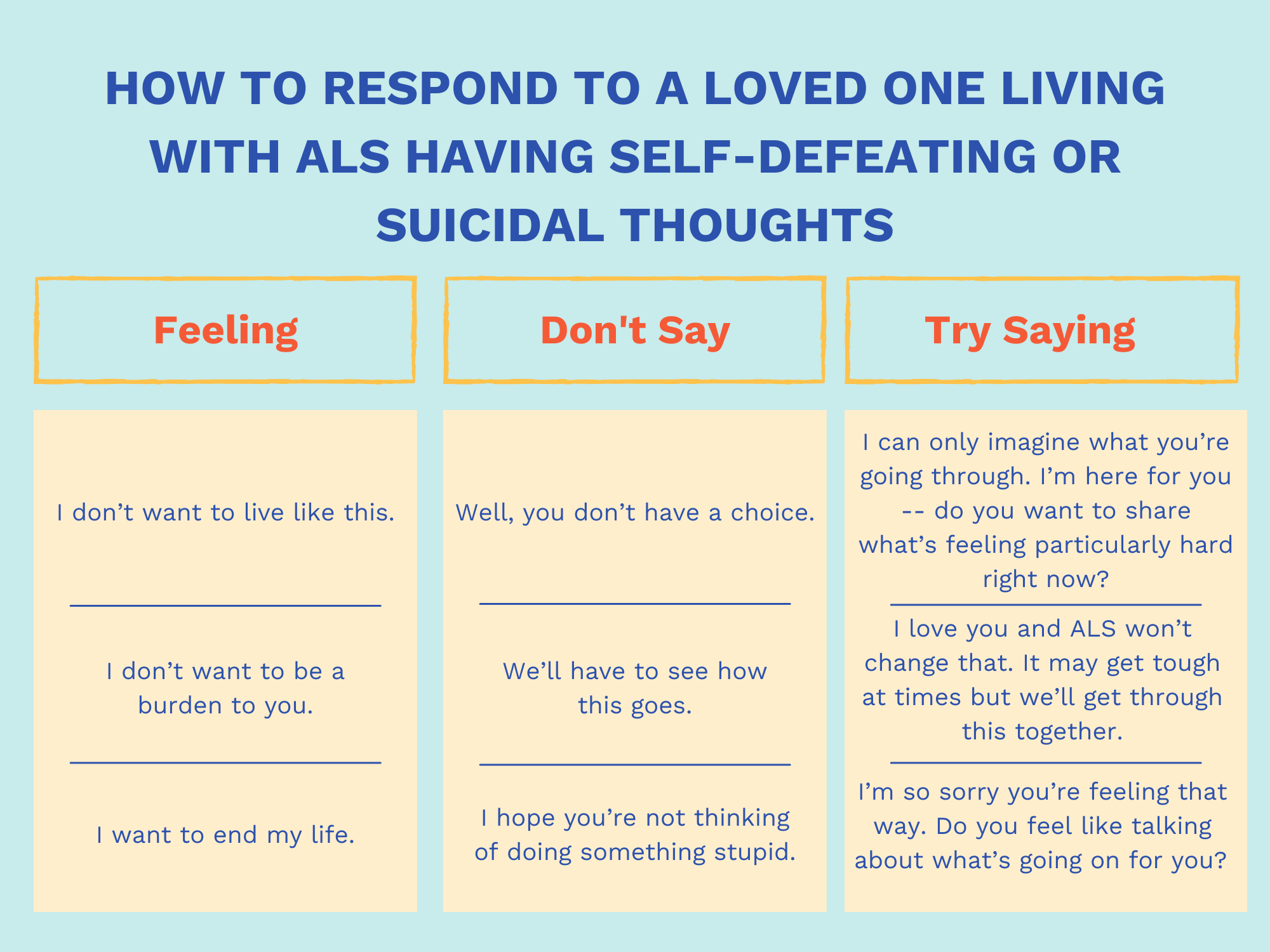
Sometimes we may have a difficult time coping with our emotions and our thoughts may spiral. All of the emotional and physical impact that ALS brings can often lead to experiencing intense feelings like “living just isn’t worth it anymore,” or “I don’t want to live like this.” You may also find yourself getting stuck in thinking that you do not want to be a burden to your loved ones, worrying about how you will pay for ALS and that you do not want to experience being in your body with ALS. These thoughts can lead to contemplations, wishes and preoccupations with death and suicide, called “Suicidal Ideation” (Suicidal Ideation, 2021).
Having such thoughts occurs for many who experience a traumatic situation. You’re not a ‘bad’ person for feeling this way, and you’re most definitely not alone. Just like trauma, suicidal ideation is different for every person, varying from the intensity of thoughts, and the duration and character of them. Even for one person, the strength and characteristics of experiencing suicidal ideation can fluctuate dramatically over time.
It is very important to recognize these feelings in yourself or another, talk about them with those you trust and get help to cope with how you’re feeling and support with other events in your life.
Harmer, B., Lee, S., Duong, T., & Saadabadi, A. (2021). Suicidal Ideation. In StatPearls. StatPearls Publishing.
Coping with Trauma and Suicidal Thoughts:
Remember, having these feelings is a valid, normal response. Once recognized, you can learn to cope with it.
Coping starts with recognition and talking about and sharing your emotions with another person, whether it be a friend or professional resource (like a therapist). Talking about these feelings over time in order to monitor them for safety is a proven strategy. Suicide ideation is considered a better predictor of lifetime risk for suicide than immediate, in-the-moment risk, so being able to look back on past suicidal feelings and current ones can be helpful for management.
Here are a few coping mechanisms that can be helpful for a person experiencing suicide ideation:
- Talk with a mental health provider (therapist, doctor, psychologist) for help with suicidal thoughts and behaviors.
- Develop intervention strategies to manage depression/mental health.
- Recognize suicidal tendencies and risk factors and eliminate them as much as possible from everyday life.
- Create a management strategy and safety plan for suicide risk when intense thoughts arise.
Resources:
If you have considered harming yourself or taking your life, please know there is help available to you.
- Crisis Text Line: Text HOME to 741741 to connect with a Crisis Counselor.
- National Suicide Prevention Lifeline: The Lifeline (1-800-273-8255) provides 24/7, free and confidential support for people in distress, prevention and crisis resources and best practices for professionals.
Caregivers:
Overwhelming feelings related to trauma, fear and shock also affect ALS caregivers and loved ones in similar ways as it affects those living with an ALS diagnosis. Seeing a person you care for choke on a bite of food, have a dangerous fall, lose the ability to do things that they once loved and need complex medical care like tracheotomy changes and feeding tubes is taxing, both physically and mentally. You may feel like you’re living in constant fear or experience high levels of stress about providing care and what comes next.
These uncomfortable feelings can be enhanced by the emotional pain of watching a person you love struggle with their mental health and have thoughts of suicide. It can feel like you’re helpless in taking their pain away, making their life more comfortable or helping remind them of their desire to live. Caregivers themselves can develop depression, mental health struggles and suicidal ideation from this trauma.
The person in your life experiencing ALS needs (and wants!) you to feel loved and supported. ALS is relentless — but so are you. This means taking time to care for YOU. Your feelings are normal and valid and there are coping strategies that can help when challenges feel too harsh to handle.
Here are just a few:
- Practice self care: Eat nutritious foods, get sufficient rest and exercise routinely.
- Pay attention to your body’s signals of stress and take breaks when needed. Pro tip: Rally your community to help make sure you get time for yourself.
- Meditate or practice breathing exercises.
- Surround yourself with friends/family by whom you feel supported.
- Find a support group.
- Talk with a counselor or therapist.
- Set healthy boundaries: Say “yes” to what you want to or can say “yes” to, and say “no” to things that are unsustainable for you.
- Connect with another caregiver for support.
We know that it can be challenging to take time for yourself sometimes because you don’t have qualified or reliable help to care for your loved one living with ALS and sometimes because you may feel guilty about leaving them to do something for yourself. Our ALS Support Team can help you by identifying respite care options for you, supporting you with processing your emotions and creating plans to get more help with care, and connecting you with other caregivers. Connect with us for support today.
Remember — The mind is a powerful muscle and can be exercised just like other muscles to create new pathways and patterns of thought. With help, you can create your own coping and management plan that allows you to work through emotions, trauma and suicidal thoughts. Remember, we are always here to listen to you, to feel with you and to offer support to you and your loved ones.
You might find these helpful:

We're here to help with the challenges of ALS
Connect with an ALS Support Specialist today
Have questions? Call us at 866.942.6257 between 9 a.m. - 5 p.m. or email us
